Design for Improving Hospital Stroke Unit Processes: Reducing Complex Systems Failures Leading to Adverse Patient Outcomes
Dr. Terence Love
Lancaster University,
Dr. Trudi Cooper
Edith Cowan
Abstract
This paper describes recent research involving a user-focused design analysis of in-hospital residential treatment for stroke patients. The focus of the research was to identify positive and negative design heuristics associated with addressing poor performance, errors and failures of patient care associated with current designs of hospital systems processes being inadequate to address actual levels of system complexity.
The research findings are based on an in–depth case study following a single patient through a stroke unit in a medium scale hospital of (approximately 280 acute beds overall) with 26 stroke unit beds. The case study involved over 200 hours of observations over nine weeks and liaison with hospital and family over the four months of the patient’s stay in hospital.
The findings suggest an explanation for the lack of effective advantage so far shown for integrated care as compared to conventional multidisciplinary care. In essence, they suggest that integrated stroke care and multidisciplinary care are both subject to similar serious systemic organisational failures that in effect reduce outcomes of both to a similar compromised position.
The paper concludes with three design heuristics for improving stroke unit outcomes via improving the design of stroke unit organisational systems. These proposed heuristics may be of benefit more widely in hospital system design for improved outcomes.
Keywords
Hospital system design, design strategies, user-based assessment, case study, viable system model.
Acknowledgements
This research was funded by Love Design and Research with in-kind support from Curtin University of Technology and
Introduction
In-hospital residential stroke support services are increasingly important because stroke are one of the major causes of disability and premature death in the developed world (NCHS, 2007; van der Walt et al., 2005). In-hospital stroke units are regarded as the gold standard in stroke care (Royal College of Physicians, 2002; van der Walt et al., 2005).Typically, in-hospital residential stroke service units bridge between initial crisis care for stroke victims and their return to the community; whether at home, in care or in a residential nursing facility (Royal College of Physicians, 2002).
Stroke units are complex socio-technical systems and they reflect the systemic complexity of the hospitals of which they are a part. Hospitals are both systemically complex and renowned for systemic errors leading to unacceptably high levels of hospital induced mortality and adverse consequences and poor treatment as reported by the Institute of Medicine (IOM) in the US (Kohn, Corrigan, & Donaldson, 1999). In the
The perspective taken in this systems-focused case study is organisational rather than clinical or medical treatment. The research used a “deep slice” approach and followed a single patient and their pathway through the hospital system from stroke at home to nursing home care. The research identified system design issues that offered opportunity for improvement in hospital services to the patient between the time of emergency admission and the time of discharge nearly four months later. Many of the identified design issues were associated with real or potential system failures or poor system performance that could be improved via design. Data collection was by informal observation of over 200 hours (over 3-5 hours of observer involvement six days a week for nine weeks) plus liaison with hospital and family members over the whole of the four months of the patient’s stay in hospital. Data analysis has focused primarily on the combined use of critical analysis and systems analysis tools of Beer’s Viable System Model (VSM) and Ashby’s Law of Requisite Variety (LoRV) with the extensions of Love and Cooper (see, for example, Beer, 1989, 1995; Glanville, 1994; Heylighen & Joslyn, 2001; T Love & T Cooper, 2007; Stockinger, n.d.). Identifying features of descriptions have been changed to avoid identifying the patient, the hospital or the healthcare provider.
Background
Stroke units are complex socio-technical systems that act as a single point of contact to combine and co-ordinate all the necessary services to support the acute treatment and rehabilitation of stroke patients (Stroke Unit Trialists' Collaboration, 2007(1995)) and have a recommended structure comprising (van der Walt et al., 2005):
· geographically defined unit
· the presence of a coordinated multidisciplinary team (stroke physician, nursing staff, occupational therapist, physiotherapist, speech pathologist, dietician, social worker and, where possible, psychologist)
· access to ongoing professional education
· regular team meetings for care and discharge planning
· use of agreed evidence-based management protocols
From a systemic perspective, stroke units fit within Individual hospitals that comprise a mix of sub-system organisations, services groups, each with differing systems and professional/work cultures. A key issue is sub-system integration and this can be of life and death importance as Kohn and colleagues identified (Kohn et al., 1999). An example is the integration of patient feeding with medical treatment in which correct feeding (including no feeding) must be matched to other clinical treatment activities such as surgery, diabetes treatment and stroke recovery.
Their complex high level of interdependencies with the other hospital systems makes stroke units potentially an ideal study for understanding and improving design of organisational systems hospital systems in general. This is particularly so as research reported by the Royal College of Physicians(2002) in Scotland has identified that stroke units sit on a boundary in which it is unclear whether, organizationally, integrated care or ‘usual’ hospital care offers the best advantages, and thus stroke units may act as a potential boundary indicator in terms of hospital organisational structures. Typically they are loosely integrated multi-service units that include: basic patient care (feeding, toileting, washing, personal support etc); medical treatment to address acute issues associated with the stroke (cerebral clots and hemorrhages as well as incidental damage from e.g. falls resulting from the stoke); physical rehabilitation services (mostly physiotherapy and speech therapy); and hospital to community re-integration services aimed at facilitating the earliest transfer of patients from (expensive) hospital care to (cheaper) community alternatives. Thus In-hospital residential stroke service units offer a useful focus for understanding and improving design of hospital systems more widely.
Stroke units are complex in five dimensions:
· Managerially complex: due dynamically shifting parallel and multifaceted webs of treatment responsibility, authority paths, patient ‘ownership’, payment and budgeting.
· Clinically complex: due to the wide variety of presentations of patients and their needs for treatment, rehabilitation and parallel management of pre-existing conditions, particularly as the relatively long hospitalization can result in secondary illness such as DVT, pressure sores, accidental injury because of falls, and depression as a secondary outcome of disability caused by the stroke.
· Administratively complex: because each of the above managerial and clinical aspects are associated with their own individual paper and electronic administration systems that overlap and integrate differently into overall National Health Service systems, as defined locally by Health Trusts.
· Informatically complex: as they act as a node receiving and disseminating patient and treatment information in the multiple dimensions of patient care and treatment that they address, including rehabilitation into community care.
· Technologically complex: relatively unusually for a hospital, the technological complexity of stroke units is primarily to do with low tech but large number of technologically based services and interactions. This contrasts for example, with the high tech found for example in surgery.
This complexity is in part due to the ‘4H’ nature of the hospital environments in which stroke units are located – high risk, high technology, high cost and high required skill. In parallel, these are essentially user-centred environments in which the focus is on best serving the patients (the users of the health system) in terms of their recovery to health. The primary intent of hospital systems is to address patients’ needs efficiently and effectively and avoid mistakes that are life-threatening, adversely affect clinical treatment outcomes, delay or reverse patient recovery, or compromise the potential for the patient to reintegrate into life outside hospital. Hospital treatment is a high cost environment compared to community care and thus must be used only where necessary. A significant aim in terms of stroke unit system effectiveness, therefore, is to facilitate the return of patients to return home or into community care as soon as possible to reduce costs.
Design of stroke unit (and hospital) systems must necessarily address two phases of patient treatment: an initial acute phase and then a stabilised treatment phase. Emergency admissions operate reactively within an environment of high variability and unpredictability to provide acute treatments. In organisational terms, this creates specific planning problems in dealing with acute situations with relatively low information determinacy, i.e. the full details of a person’s illness are often not available. After the initial crisis response, however, organisational systems should proactively facilitate a patient’s progress through the system and the patient’s eventual discharge into community-based care.
The case study below reviews the organisational systemic issues relating to a single case of a patient admitted as an emergency to a hospital with symptoms of collapse and unconsciousness. The treatment pathway was that of stroke assessment and rehabilitation. The central component of the study is of the systems of the in-hospital stroke unit. The study below:
- Describes a real life case
- Identifies potential for systems design improvements
- Identifies potential for improved design strategies
The benefits of undertaking a case study following a single patient through the system, rather than (say) using aggregate data across many patients, are that it reveals specific systems failures and links them to their antecedents; it offers the opportunity to ask in the moment, ‘how could this system be designed better?; and it reveals and identifies in a concrete way specific design opportunities that follow from particular real world events that are part and parcel of being a hospital user.
Case Study – Elderly Man Treated for Stroke via In-Hospital Stroke Unit
Michael was an elderly man admitted to hospital following a major stroke. Admission was by ambulance directly to the Accident and Emergency Department. He arrived mid-morning. Following triage he was transferred to the Medical Assessment Unit (MAU) to await placement. He remained there for two nights. It is unclear whether standard recordings were kept, but these could not be found some weeks later when they were requested (design issue).
The MAU acted as a holding bay for patients awaiting test results that determine treatment and identify the appropriate specialist ward (design issue). Tests confirmed a major stroke. Michael was aphasic, unable to swallow and suffered hemi-paralysis.
The stroke unit had no spare beds. Michael was placed in a male medical ward (design issue). Because Michael was immobile, his relatives inquired about what nursing precautions were being taken to prevent bed-sores. They were told that no pressure relieving mattresses were available and nursing care would ensure he did not develop bed sores (design issue). The medical ward was geared to the needs of patients recovering from surgery, but actually included patients with a variety of needs, placed there because beds were not available in wards more appropriate to their needs (design issue). Staff did not have good understanding of the needs of non-surgical patients, e.g. all patients were dressed in hospital gowns rather than pyjamas, as a matter of course (design issue). Aphasic patients were assumed unable to understand and staff did not talk to Michael, reassure him, explain procedures or seek his consent (design issue).
Patients’ names were written on a whiteboard. To avoid medication confusion, an asterisk was placed by the names of patients who shared the same family name. The researchers noticed that two pairs of patients shared the same family name, but only three patients had asterisks by their names. One of the four patients had been missed (design issue).
Before Michael left the surgical ward, he developed a sore on the heel of his immobile leg. A pressure relieving mattress was eventually located after his relatives drew attention to his need (design issue). The sore was not fully healed when he was discharged from hospital over three months later (design issue).
After a stay of three nights a bed became available in the Stroke Unit and Michael was placed in a single bedded ward in the acute section. He remained there for just over two weeks. The wards had a hand basin to enable staff to wash their hands as an infection control measure. Infection control in
Michael was assessed and found to have a weak swallow reflex (and hence might choke on food) but could be tried on ‘tasters’ of thickened fluids and pureed food in small amounts. The weakness of his swallowing reflex meant that he could only be fed by trained nursing staff. He slept a lot, a side effect of a stroke, but feeding could only occur when he was not drowsy. His meals would arrive and a trained staff member would sometimes look in to see whether he was awake. If he was not awake or if no trained staff member checked, his meal was removed, even though a few minutes later he might wake up and be able to be fed (design issue).
At this stage, Michael had not eaten for over a week, during which time he had received two gastro-nasal feeds and visibly lost weight. Initially, Michael had very little appetite but later his appetite returned. On many occasions when Michael was awake and food was served, no trained member of staff was available to feed him and he had no food. Four weeks after his stroke, he had lost 15kg and looked emaciated (design issue).
Three weeks after Michael’s stroke, he was started on physiotherapy on a daily basis. At this time, he was still rarely getting sufficient food and he appeared tired and weak and confused. The physiotherapists decided that he was not making rapid progress and decreased the frequency of physiotherapy. The physiotherapists knew that Michael had problems swallowing and lost weight but reinterpreted the situation as ‘slow neural recovery’. This had important consequences because it reduced what is regarded as an important component of stroke treatment (design issue).
A case conference scheduled two months after admission occurred two weeks late. The various specialists (speech therapist, physiotherapist, care manager, nurse, the doctor did not attend) presented their findings from tests and assessments. The reports suggested Michael had made little recovery and it was suggested Michael would need nursing care and should be eligible for financial support. (In this jurisdiction, under some circumstances, severely disabled people are entitled to financial support for nursing home fees.). Relatives were advised they would be notified about Michael’s eligibility for financial support for a nursing home on a specific date within two weeks.
Financial considerations are an important issue. Public financial support pays for most of the costs of residential nursing care. Otherwise the relatives have to pay up to £1000/ week for the care. This contrasts with the public cost of £1000/ day for hospital care. The researchers noted some stroke victims remained in hospital for extended periods over and beyond that needed for hospital treatment because of lack of funding for the patient to move into residential nursing care. This is in spite of the 700% additional public costs to retain them in hospital (design issue).
Michael’s relatives were advised to urgently look for a vacancy in a nursing home. They were advised that high quality Nursing home places are difficult to find and usually filled from a waiting list. The relatives found a nursing home place and agreed for Michael to move there. The nursing home agreed to hold the place until the date of the decision about financial support. The financial decision, however, was delayed because Michael’s case had not been presented. It transpired that the relevant paperwork had not been signed by key staff (design issue). The nursing home agreed to hold the place for a further week. The arrangement to make the financial ruling failed on a further two occasions, with different hospital staff providing different explanations and excuses (often contradictory) (design issue). This resulted in very high levels of stress on Michael’s relatives (and Michael)..
The nursing home was not able to retain an empty bed and Michael’s relatives were placed under considerable pressure by hospital management to agree to Michael being discharged from hospital before resolution of the financial issues.. There were multiple problems with the inter-professional communication and integrity of this process (multiple design issues). On one occasion the relatives were assured by the care manager that financial support had been agreed, only a few minutes after nursing staff said his financial case had not been considered by the panel, only to be told a few hours later the care manager had made a mistake (design issue). After the third delay, Michael’s relatives were assured it would not prejudice the outcome of the financial decision if Michael moved into the nursing home and, under pressure from both the hospital and nursing home, the relatives agreed to Michael’s discharge into the nursing home. A few days after Michael’s discharge from hospital the relatives were informed Michael’s case for financial support had been rejected.
This placed Michael in an impossible position in terms of getting necessary nursing care. At this point, Michael needed high dependency care, could not communicate, and had a thrombosis in one leg. The extent of Michael’s abilities was to move one arm and apparently to understand conversation (he could nod and shake his head). It was unclear how he would manage without nursing support. On appeal, after considerable effort by the relatives, the financial ruling was overturned and nursing care was funded.
Michael’s limited physical condition meant he needed sitting support. In hospital this was provided by a specialist chair designed with adjustable support arrangements to hold stroke patients' bodies upright (an important part of recovery). These chairs are normally provided by the health services. Michael’s relatives asked about how they would obtain a suitable specialised wheelchair and armchair for Michael. This triggered a wheelchair assessment process during which it transpired that Michael also needed a custom made wheelchair to be provided by the hospital but would take between two and six months to be made available (design issue). It arrived eight weeks after Michael’s discharge. However, it nearly didn’t arrive at all because the wheelchair service had no record where Michael had been sent on discharge and only discovered as a result of relatives contacting them (design issue).
Michael also needed a special armchair (paid for by his relatives) that took nearly three weeks to arrive. Assessment occurred only in response to relatives’ requests, and occurred too late for Michael to have the correct equipment on discharge. No process was put in place to inform relatives of the likely timescale or to ensure that assessment was completed to allow time for fitting, manufacture and delivery (design issue). It is not clear whether any assessment would have taken place at all if the relatives had not been persistent. In the end, Michael was discharged without either a wheelchair or his custom armchair as a result of failures of communication, faulty system processes and unplanned and unmanaged delays in the stroke unit systems (design issue). That the process worked at all was due to persistent proactive efforts by Michael’s relatives.
During the time of observation, it was clear that most staff were working beyond what could reasonably be expected. Many were working beyond their hours in an attempt to rectify problems that were caused by the failing of hospital systems.
Design issue themes
Of the design issues identified in the case study, some are abstract, some concrete, some organisational, some structural, and some to do with the design of individuals’ behaviours. They can be clustered under the following themes:
· Communication processes
· Differences in Professional assumptions and practices
· Poor system integration (this may actually be a system of systems problem rather than a single system problem. However, diagnosis and designed solutions are similar in both cases)
· Local suboptimisation. This occurs when a functional group, which may be an individual, optimises its tasks for the benefit of itself at the expense of the overall system.
· Confused management processes. This design problem appeared common and often occurred when either a single individual has multiple managers who each have a claim on their time, or where multiple functional units or staff (e.g. nursing, food supply, physiotherapy, neurology, community care coordinator) are all necessary to a satisfactory completion of a task and yet this depends on individual decisions by their managers, whose focus is in optimising the functioning of their own cost centred area.
· Non-medical client services.
· Significant tensions between crisis medical care and ongoing medical systems
· Weak integration of community care and transition to community care with medical services and hospital care services.
· Poor transitional arrangements. This design issue was observed to occur across all dimensions and systems. It occurred at the boundary between the community and hospital systems; at the transition between acute care and the medical ward; at the transition between the medical ward and the short term-acute stroke care; and at the transition form acute stroke care to rehabilitation ward. It also occurred in multiple dimensions of the transitions between in-ward nursing care and in- ward physiotherapy services and at the transition between in-hospital care and community care, in Michael’s case, his transition to a Nursing home.
· Weak integration between hospital strategic planning and lower level processes both at the level of individual patient care services and, above that, in the provision of professional specialist services, and the management of both sorts of services.
· Care co-ordination and professional staff. During the case study we observed professional behaviours that compromised the bigger picture of hospital services as a temporary health support for individuals to be able to return to normal lives in their community. These problem behaviours primarily appeared to be related to underlying systems problems and in some cases appeared officially sanctioned to address systems failures. In one instance, a nurse who had been recently demoted because of lack of competence in distributing medicines was performing many duties normally assigned to trained staff. The reasons that she had been demoted were overlooked for local suboptimisation in terms of reducing costs or addressing staffing mismanagement.
· Staff, especially trained nursing staff, were often unable to complete their work in the time available. Some stayed on at the end of their shift to try to catch up, even though they did not get paid overtime. Other staff complained about the pressure they felt under and stated that this erode their sense of job satisfaction. For some staff alcohol abuse seemed to be an issue. According to Cary Cooper, this is often symptomatic of unsustainable staff stress (Cooper, 1998).
· Ongoing multidimensional tension between hospital management processes and the management of specialist professional liability and risk
· Ongoing overwork of staff in the main to rectify problems intrinsically caused by problematic designs of hospital systems. Classically, this latter is a management issue rather than a failing of workers (Deming, 1986).
Discussion
Many of the above design issues are closely related to weakness in the integrity of decision-making processes whereby many decisions have multiple dimensions in integrated situations and are delegated to specialists who are have a limited focus that does not include the other dimensions of integrated service provision. This is a core design issue and applies whether a hospital applies models of integrated care or multidisciplinary care.
Currently, the hospital system primarily comprises two contradictory systems:
· Specialists with highly focused specialist knowledge and bounded knowledge and responsibilities (this is to avoid specialists acting outside their expertise in ways that might lead the health service to be subject to litigation and legal charge of incompetence)
· A health provision situation that requires complex integrated multidimensional services responses across a variety of specialist functions.
Attempts to resolve this systemic contradiction follow two paths: 1) multidisciplinary case meetings; and 2) specialist integration managers whose responsibility is to manage the integrated care of a patient. Our observation is that both approaches fail to the extent that the overall system fails. It was inferred from observation that a primary reason these approaches failed to provide integration is because of the embedded culture of reification of specialists. This is particularly evident in the system tensions between acute, crisis medical care and longer term care. It occurs in different forms. In acute crisis care, integrated responses appear to be subsumed to ‘addressing the crisis of the moment’. In longer term medical care, the failure occurs because the attention is to maximise the efficacies and reduce Coasian transaction costs of day to day care processes in which integration systems are regarded as an add-on to be deferred or ignored. The weight of time, effort and attention is on the habituated delivery of routine services of feeding, medication delivery, toileting, and managing visitors.
Systems Design – Viable Systems and Ashby
In design terms, many of the above design problem themes can be usefully interpreted via Beer’s Viable Systems Model and Ashby’s Law of Requisite Variety as extended by the authors.
In system terms, most of the above design problem themes can be located on Beer’s Viable System Model (Beer, 1972, 1988) as shown in Figure 1 below.
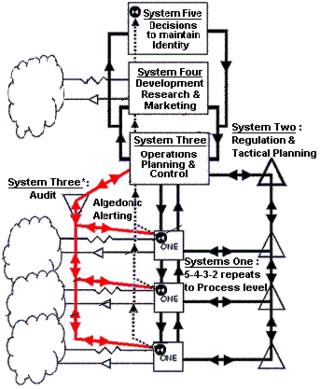
Figure 1 Viable System Model (Green, 2007)
Beer’s Viable System Model (VSM) shows the essential elements and relationships needed by any system to be viable and function successfully. A viable system comprises five main subsystems.
Systems 1 are sub-systems that interact directly with the external environment (represented by the ‘clouds’) to undertake the main purposes of the overall system. Typically, there are several. In the hospital systems these Systems 1 include all the subunits that support patient medical treatment and care such as specialist doctors, surgery, physiotherapy, feeding, ward cleaning services, patient records administration, patient transport systems etc Each System 1 is also a complete system – the VSM is recursive.
System 2 comprises the processes by which Systems 1 interact and are monitored and coordinated by System 3.
System 3 is an intermediate management sub-system between Systems 1 and Systems 4 and 5. It comprises all that is necessary to direct Systems 1 (rules, rights and responsibilities) and to monitor and manage Systems 1. In the hospital system, System 3 is undertaken by managers at the level of ward sister. System 3 also includes an algedonic loop to manage rapid change of crisis and failure. Note: this is crisis and failure of the system – not the patient.
The focus of System 4 is gathering information from the external environment. In the hospital system, this is information such as the needs of the constituencies that the hospital supports, new medical technologies and improved ways of designing hospital systems. System 4 provides evaluation and forecasting information to management systems 3 and 5.
System 5 provides overall policy and strategic guidance for the whole organisation. This is typically the role taken by the hospital board and senior administrators. For a more detailed description see, for example, Beer (1989; 1995) and
Where an organisation is designed such that any of the VSM functions are missing or weak then a range of typical organisational pathological developments occur. Several of these characteristic pathologies can be seen in the list of design problem issues and themes that emerged in the case study.
In this case study, three particularly obvious system problems that relate to the above design issues are:
1. Multiple Systems 3 which are themselves uncoordinated and have weak line management and information flow relations with Systems 2, 4 and 5. The consequence are failures of management confusion, faulty integration of services, and flawed transitional arrangements that typify most of the design issues identified earlier.
2. Reification of some Systems 1 (doctors and specialist medical personnel) such that they are tacitly and sometimes explicitly locally given the status and line management of Systems 3, 4 and 5. This results in complete failure of integrated management of the system.
3. Attempts to superficially remedy the problems of failure of System 3 by overemphasis of System 2. That is, to requires some Systems 1 to be subjected to high levels of self reporting to management. This fails on a number of counts, the most obvious being that System 3 is weak and unable to fulfill its role. An additional effect is that it results in System 3 responsibilities being pushed down to individual Systems 1. Again this destroys the primary functioning of the System 3 role of providing integrated management of Systems 1.
Applying Ashby’s Law of Requisite Variety echoes this picture. In a hospital system that is operating in an organisationally healthy manner, the primary generator of variety is the patient. System variety is primarily generated via their illness and related issues (e.g. missing work, managing children etc). The hospital acts as a system of controlling variety in which the variety due to the patient’s illness is attenuated in an appropriate manner such that the patient can leave hospital and as much as possible resume their life.
The case study reported a situation in which the largest generators of system variety are the hospital systems themselves. Much of this extraneous system variety is in the form of defects caused by failures of integrated response in the control variety generating systems causing problems that must then be addressed. Examples of this in the above case are the failure of integration of patient feeding processes, the failure of case meetings and the failure of the community care and in-community care funding decision making processes. These defect and failures of system design resulted in additional work to respond to the patient’s relatives, providing additional hospital services to the patient because of the earlier failures compromised the patient’s recovery; and redoing of administrative and decision making processes with additional layers of paperwork. In systems terms, many of these issues are caused by mismatch in the distribution of the generators of system variety and control variety driven by local subsystems’ attempts to manipulate the system to gain additional power, status and resources (Glanville, 1994; T Love & T Cooper, 2007; T. Love & T. Cooper, 2007).
These issues are also addressed by Deming’s (1986) classic work on quality management where he describes the central importance of designing systems so as to primarily reduce defect generation. In the case of the hospital system observed in this case study; defect generation is high and mainly comprises failed provision of integrated services or failures in transition of the patient and patient control between sub-systems. In essence, these failures are primarily generated by the hospital systems themselves and align with the diagnosis from Beer’s Viable System Model and the variety analyses.
The analyses above contradict and explain the implications of findings of Sulch and colleagues (2000) who found no differences in outcomes between integrated care and conventional multidisciplinary care models of stroke treatment and suggested the advantage lay with the conventional multidisciplinary care is resources did not need to be allocated to the person undertaking the integration. The findings of this research suggest that the significant potential benefits attached to the use of the integrated services model over multidisciplinary care will only be available with resolution of the systems problems identified above
The observations of this research suggest that the outcomes of both integrated care and conventional multidisciplinary care are deeply compromised by systemic organisational problems. The ‘deep slice’ systems analysis used in this case study suggests that all hospital processes are likely to be significantly compromised where they involve supplying multiple services to a patient due to the systems exhibiting the pathologies of a compromised viable system as per Beer’s VSM. These systemic pathologies would be expected to cut away the potential advantages of the integrated stroke services model and reduce outcomes to similar to conventional multidisciplinary approach as found by Sulch (2000). The implied opportunity to improve stroke unit outcomes is to resolve the serious systemic issues first and then move to an integrated stroke service model.
Conclusion – three design heuristics to improve design of systems for hospital stroke units
The above case study has identified and analysed design issues in a hospital stroke unit in terms of systems design using three approaches. The analyses indicate significant opportunity for improved design of the hospital’s systems.
Some design issues appear foundational: addressing systems integration; dealing with transitions; and addressing the contradictions between specialist professional services and management of integrated service delivery. When the systems are mapped to the VSM, the observed problems align directly with the predictions of organisational pathologies.
The three analysis approaches suggests three design heuristics in creating improved design solutions for the stroke unit. These would also be expected to apply more widely across other hospital systems and hospitals:
1. Review existing hospital systems in terms of the Viable Systems Model to identify structural problems in systemic design, and design new systems to address these structural problems
2. Focus design resources on supporting management to address provide significantly improved support for fully integrated care provision. This means developing designs that will in parallel support specialist professionals in avoiding liability whilst acting against the current culture of inappropriate reification of specialist professionals.
3. A focus on integrated care at organisaitonal transition points. This requires all dimensions of patient care, community issues care and medical care to be managed in an integrated manner when the patient is transferred into and out of the hospital and within the hospital from one subsystem area to another.
The case study suggests that targeting these three areas of design will place the focus on the lever points of addressing the primary areas of systems failure. In addition, it would be expected that addressing these issues will also incidentally address most secondary systems issues and open up the potential for gaining the benefits of integrated care over multidisciplinary care.
References
Beer, S. (1972). Brain of the Firm. London: The Penguin Press.
Beer, S. (1988). Heart of Enterprise. Chichester: John Wiley and Sons Ltd.
Beer, S. (1989). The Viable System Model: its provenance, development, methodology and pathology. In R. Espejo & R. Harnden (Eds.), The Viable System Model: Interpretations and Applications of Stafford Beer's VSM. Chichester, UK: John Wiley & Sons.
Beer, S. (1995). Diagnosing the system for organizations. Chichester: Wiley.
Cooper, C. L. (Ed.). (1998). Theories of Organizational Stress. Oxford: Oxford University Press.
Deming, W. E. (1986). Out of the crisis. Cambridge, Mass: Massachusetts Institute of Technology and Cambridge University Press.
Glanville, R. (1994). Variety in Design. Systems Research, 11(3), 95-103.
Green, N. (2007). VSM figure. In Vsm.gif (Ed.) (Vol. 343 x417 pixels, pp. Diagram of Viable System Model (VSM) of Beer): GFDL and wikipedia.
Heylighen, F., & Joslyn, C. (2001). The Law of Requisite Variety. from http://pespmc1.vub.ac.be/REQVAR.html
Hutchinson, W. (1997). Systems Thinking and Associated Methodologies. Perth, WA: Praxis Education.
Kohn, L. T., Corrigan, J. M., & Donaldson, M. S. (Eds.). (1999). To Err is Human: Building a Safer Health System. Washington, D.C.: Committee on Quality of Health Care in America, Institute of Medicine and National Academies Press.
Love, T., & Cooper, T. (2007). Digital Eco-systems Pre-Design: Variety Analyses, System Viability and Tacit System Control Mechanisms. In E. Chang & F. K. Hussain (Eds.), 2007 Inaugural IEEE International Conference on Digital Ecosystems and Technologies 21-23 February 2007 Cairns, Australia (pp. 452-457). Los Alamitos, CA: IEEE.
Love, T., & Cooper, T. (2007). Successful Activism Strategies: Five New Extensions to Ashby. In K. Fielden & J. Sheffield (Eds.), Systemic development: local solutions in a global environment. ANSYS 2007 proceedings (Vol. [CDROM]). Auckland: Unitech.
NCHS. (2007, 31 Dec 2007). Stroke/Cerebrovascular Disease. Retrieved Jan 2008, 2008, from http://www.cdc.gov/nchs/fastats/stroke.htm
Royal College of Physicians. (2002). Management of Patients with Stroke Rehabilitation, Prevention and Management of Complicaitons, and Discharge Planning. A National Clinical Guideline. Edinburgh: Scottish Intercollegiate Guidelines Network.
Stockinger, G. (n.d.). The Role of Variety in the Evolution of Information Society. from http://kaneda.iguw.tuwien.ac.at/stockinger/fis.htm
Stroke Unit Trialists' Collaboration. (2007(1995)). Organised inpatient (stroke unit) care for stroke [Electronic Version]. Cochrane Database of Systematic Reviews, 2. Retrieved June 2008 from http://www.cochrane.org/reviews/en/ab000197.html.
Sulch, D., Perez, I., Melbourn, A., & Kalra, L. (2000). Randomized Controlled Trial of Integrated(Managed)Care Pathway for Stroke Rehabilitation [Electronic Version]. Stroke, 1929-. Retrieved June 2008 from http://stroke.ahajournals.org/cgi/content/full/31/8/1929.
van der Walt, A., Gilligan, A. K., Cadilhac, D. A., Brodtmann, A. G., Pearce, D. C., & Donnan, G. A. (2005). Quality of stroke care within a hospital: effects of a mobile stroke service. eMJA, 182(4), 160-163.